The shift to value-based care is just one of many fundamental changes happening in healthcare today. Healthcare organizations across the continuum are challenged to increase productivity AND reduce costs while maintaining proper staff levels to meet patient needs and compliance requirements. Hours per patient day is a common industry expression used to trend the total number of direct nursing care hours , compared to the number of patients as the HPPD ratio. Using a the "nursing hours per patient day" is a way to monitor and improve quality of care and service. And in many states, hospitals, clinics, acute care facilities, long-term care and senior living facilities must report the HPPD data to the Department of Public Health. The panel reviewed current staffing ratios of registered nurses, licensed practical nurses, and nursing assistants, and concluded the current levels are inadequate.
Seventeen out of the 30 conference participants endorsed a final staffing recommendation that established 4.55 total nursing hours per resident day as a minimum threshold. Noting that nursing management and leadership are central to providing a high quality of care in nursing facilities, the panel also recommended the director of nursing in nursing facilities have a minimum of a bachelor's degree. Since 2012, University College London Hospitals Foundation Trust has set ward nursing establishments using the SNCT.
The executive board is given regular updates on nursing and midwifery staffing and patient outcomes and experiences of care. Data on patients' levels of sickness and dependency is collected and analysed three times a year. The ward sister, matron and head of nursing review staffing and the data alongside nurse-sensitive indicators , using their professional judgement to put staffing proposals to the annual staffing review. Agreed changes to the establishment are reflected in the following year's ward budget and updated on the e-rostering system. This allows recruiting to new posts and adjusting of "planned hours" of nursing care by day/shift for each ward. Any discrepancies between establishments, patient outcomes or experiences of care and nurses' professional judgement triggers an external service review.
If there is one registered nurse fewer than rostered, nurses are each caring for more than seven patients, or there are "red flag" events , the nurse in charge follows a standard escalation procedure, ultimately reporting to the chief or deputy chief nurses. NSIs are reviewed at monthly meetings of the matrons and nursing and midwifery board, allowing process and outcomes measures sensitive to nurse staffing to be monitored. A mobile app allowing direct data input on the ward has reduced time spent on data collection for each ward by 45 minutes a day. OSHPD's Hospital Disclosure Report measures employment in terms of productive hours for each of RNs, LPNs, unlicensed aides/orderlies, management and supervision, administrative and clerical, and other labor categories. Most hospitals use their payroll system, not their actual unit-level staffing grid, to complete the survey, and thus the data are subject to errors that might exist in any payroll system.
For example, hospitals might not consistently measure hours worked by nurses normally assigned to one unit but "floated" to another. The number of patient days or services provided in each revenue unit is reported, enabling calculation of hours per patient day, hours per patient discharge, and/or hours per service provided. Unit types can be aggregated or examined separately (e.g., HPPD for medical–surgical acute care only). In this study, patient care, patient transfer out hospital, and cardiopulmonary resuscitation were identified as the workload components of the nurses' main activities. In the quality-activity-dependence-based nursing staff planning, it is assumed that patient dependency is a precise scale of patient's need for nursing care, and the need for human resources based on patient dependency has a relatively high accuracy . In Western Australia, nursing hours per patient day are used as a priority in determining the need for nursing staff .
In this study, the transferring patients are another part of the nursing workload. Patient transfer is inevitable and is a part of the treatment process , which is intended to improve the provision of health services and reduce mortality and disability in patients . In Iran, given the patient's condition, the trained nurse is designated as a member of the patient's transfer team in consultation with the referring and receiving physician .
Hence, given that a relatively large number of patients are transferred to other health facilities to receive higher-level services, this has led to a great pressure for the health system including excessive use of human resources, especially nurses. Frimley Health Foundation Trust has used the SNCT throughout the trust to decide on nurse staffing levels for the past four years. Data on patients' levels of sickness and dependency is collected three times a year but the trust is now considering daily use of the tool, to ensure staffing needs based on patients' level of care become part of the daily "currency" of care. As the tool does not take into consideration the turnaround of patients in the emergency department, so the trust no longer uses the tool in these areas. However, a recently adapted version of the tool is now used for the trust's acute assessment units. The trust gained the cooperation of staff by involving nursing staff from the outset, and encouraging open discussion of the advantages and disadvantages of using the tool.
The senior sisters lead use of the tool, and data for each ward is collected by three people, either the senior sisters or a nominated deputy, One of the biggest challenges has been validating the data and ensuring consistency. Once a week when data is being collected, the trust allocates two senior nurses, one external and one from the ward, to validate and peer review the collection. Senior nurses also receive training three times a year prior to data collection, using case studies to agree the level of care. The tool lets the trust decide nurse staffing on the levels of care needed. The director of nursing is now proposing to use the data for budget review. Correlations between the AHA and OSHPD datasets for inpatient days and RN employment were high overall, at least 0.9.
The means of RN and LPN employment were not statistically significantly different, while computed hours per patient day were statistically different in the OSHPD and AHA datasets. Most hospitals provide the staffing data to OSHPD and AHA from payroll systems, which might contain several types of measurement error. First, these systems do not delineate direct patient care from nondirect care in productive staff or hours, and thus overestimate the amount of direct nursing care received by each patient.
For example, a nurse might change the unit to which s/he is assigned, without a change in pay, and this change may not be reflected in the payroll data in a timely fashion. Nursing staff planning is of central importance because of the governments' commitment to patient safety and quality care, as well as the link between nursing workload and patient care quality . In a health care system, among the clinical staff, nurses, who generally account for more than 50% of the total staff in a hospital, play the most important role in promoting community health . Therefore, the provision of desirable care services depends on the quantitative and qualitative development of nursing staff.
Care Hours Per Patient Day Calculation Qualitative development of nursing care is achieved through continuous education, material and spiritual motivation, monitoring, and evaluation of nursing activities. On the other hand, the quantitative development of nursing staff are obtained through the use of appropriate estimation norms of nursing staff and on time supplying and distribution of them in healthcare facilities . A guideline from the National Institute for Health and Care Excellence and a NICE-endorsed tool on safer nursing care allow decisions on safe staffing levels to be made at a local level.
Decisions must be based on sound evidence and factoring in patients' individual needs as well as numbers of patients. The Safer Nursing Care Tool helps nurses decide on safe nurse staffing for acute wards based on patients' level of sickness and dependency. It also includes quality indicators linked to nursing care to help ensure staffing levels achieve best patient care. The tool is easy to use by frontline nursing staff, but must be applied correctly and consistently for data to be valid, and to allow benchmarking against agreed standards. It should be combined with nurses' professional judgement and account for local factors.
Many researchers and health care leaders want to measure nurse staffing according to the workload of each nurse, although "workload" does not have an agreed-upon definition. Most hospitals can easily report the average number of productive nursing hours per patient day ("hours per patient day" or HPPD), because they keep data on nursing hours and patient days. We modelled the relationship between staffing deficits and nurse-reported measures of staffing adequacy.
For this we used the first available SNCT rating per day for the proportions of patients in each level, the 7am patient count,actual staffing and patient hours from 7am-7am, and the staffing adequacyrecorded in the morning of the next day. We fitted multilevel logistic regression models for binary outcomes using the glmer function from the lme4 package29 in R. All models included control for day of the week, proportion of single rooms, turnover and unit specialty . We considered the association of staffing adequacy outcomes with deviation of both registered nurse staffing and nursing assistant staffing from their estimated requirements.
In acute care hospitals, the ability to determine the 'right' number of nursing staff to employ and to deploy on any given shift is an imperative, as nurse staffing levels influence both efficiency and quality of care delivery. On the one hand, professional nurses and nursing support staff form the largest group of staff and the largest variable costs faced by hospitals. We explore the reliability and precision of the estimates of required staffing establishments made using the tool and the extent to which estimated staffing requirements correspond with professional judgement of sufficient staffing.
Despite the tool's widespread use and the importance of these considerations, these factors have not been previously studied. Based on an analysis of 1999 cost report filings, all of Connecticut's nursing facilities licensed as CCNHs exceed the minimum nursing-staff-to-resident-day ratios established under the regulations. Although the regulations require 694 annual minimum nursing staff hours for CCNHs, all nursing homes licensed under the CCNH category had 754 annual hours or more per bed in direct care staffing. Based upon the data contained in the cost reports, there was an average of 1,435 direct care hours per resident per year; more than double that required under the regulations.
Reasonable arguments could be made to reconsider HPPD as a primary measure of nurse staffing for quality of care studies. While HPPD can be calculated from available data sources, this measure suffers from inadequate consideration of actual nursing care required for hospitalized patients. Nor does HPPD address completely the use of non-nursing assistive personnel. It is more accurate, however, than using an HPPD measure restricted solely to registered nurses, which can be calculated from administrative data sets on national samples.
Moreover, measures using HPPD require noteworthy assumptions for calculation, and comparison across personnel classes is challenging. The issues of staffing adequacy and in particular, the sufficiency of assistive personnel are not captured easily in administrative data. However, these important factors can be measured through questionnaires to nursing personnel. In contrast, data collection from personnel surveys suffers from cost, response rate, and logistical challenges.
The result of a study can be used as a tool for auditing the distribution of nurses throughout the country. The use of required nurse estimation norms based on the workload indicators along with eliminating the intuitive decisions of managers can be considered as an effective strategy to improve both nursing staff and patient care levels. Briefly, planning for nursing personnel can be done using WISN method for proper allocation and deployment; therefore, the workload can be distributed among nursing staff in all hospitals to improve the health care services. The program review committee believes the minimum nursing staff ratio suggested in HCFA's study is based on the most comprehensive and defensible research to date.
Furthermore, the establishment of minimum nursing staff standards does not negate the federal and state requirements that nursing facilities provide adequate nursing staff to meet residents' needs. Minimum staffing thresholds merely establish a floor below which a facility cannot drop. The program review committee compared the minimum regulatory nursing staff requirements to actual hours of nursing staff reported by facilities in its Medicaid cost reports. There are several caveats attached to the data used for an analysis of the distribution of nursing staff among Connecticut's nursing facilities. First, the number of hours reported for RNs, LPNs, and nurse aides by facilities is self-reported and not audited by DSS.
In addition, there are no uniform definitions for reporting on nursing staff hours. Thus, while some facilities may report paid hours, which include any vacation, sick, and personal time accrued, others might report actual hours worked. Third, nursing staff hours are reported on an annualized basis, but daily, weekly, and monthly nursing staff fluctuations may vary considerably. Finally, data were available for only 226 facilities out of the 253 licensed CCNHs, and estimates are based on an average 95 percent occupancy rate, rather than a facility's actual occupancy. Some researchers have argued that hours per patient day is the most precise measure of the amount of nursing care provided to patients (Budreau et al. 1999).
However, hours per patient day do not accurately measure the impact of admissions, discharges, and transfers on the workload of nurses. Unruh and Fottler have demonstrated that nurse staffing measures that do not adjust for patient turnover underestimate nursing workload and overstate RN staffing levels. While prospective unit-level databases such as CalNOC often include measures of admissions, discharges, and transfers, administrative databases do not include such measures. The survey requested that hospitals provide data for a representative medical–surgical unit in the hospital.
Survey questions focused on nursing hours worked on that unit, discharges and patient days on the unit, nurse-to-patient ratios, number of vacancies, and average time to recruit a RN to the unit. Both hours per patient day and the nurse-to-patient ratio were reported directly by unit managers, enabling a direct comparison of these methods of measuring nurse staffing. Table III-I describes the minimum nurse and nurse aide staffing requirements for CCNH and RHNS beds in Connecticut. The regulations establish minimum standards for nursing-staff-to-resident ratios during two segments of a 24-hour day and are expressed in terms of staff hours per patient . For example, on average the regulations require each resident receives 84 minutes of total nurse and nurse aide care during the 7 a.m. Since the WISN method uses the annual service statistics to measure workload and the accuracy of the WISN method and results are determined by the accuracy of the statistics, if the statistics have not been recorded properly, then WISN results will be in error.
Moreover, the WISN method uses the statistics of healthcare services of the last year; therefore, this method calculates the number of the workforces that was needed for last year. This is not usually a serious and disturbing issue due to the slow changes in the workload of health care centers in line with demographic changes and economic conditions. To solve this problem, the latest and the most current workload information was used. Occasionally, the lack of medication or supplies reduces the workload of a facility.
In the present study, it was tried to reduce the effect of this problem by selecting educational and non-educational hospitals with desirable nursing care. Another limitation of this study was that our observations might have been affected by the human error or violations in measuring the time. Since selected nurses were responsible for this type of measuring in the work study, this effect was negligible. In this work, only hospitals affiliated to MUMS were studied which makes it difficult to generalize the results to other hospital throughout the country. Considering that the average time of nursing care rarely varies in the same sectors and since the hospitals with the highest level of care were considered in the present research, this issue was not a concern.
The last limitation of the study was the fact that we relied on experts' views to estimate some activity standards; this might have affected the precision of the estimation. The current minimum total nursing staff hours per resident in a CCNH bed is 694 hours annually. This means each resident can expect to receive 13.31 hours of direct care each week. Figure III-1 shows the minimum number of nurse and nurse aide hours required per- resident-day is 1.9 hours - an average of less than five minutes of care per resident, per hour.
In terms of licensed nursing personnel for a CCNH, the minimum requirement is .64 hours per day. If nurse aides provide all of the non-licensed care that is allowed, they will provide a total of one hour and 16 minutes of care per resident each day. Decisions about the adequacy and appropriateness of nurse staffing have long been based on functionally outdated industrial models that focus on work sampling and time-and-motion studies conducted in semi-simulated settings. Even today, the common method of staffing nursing units or identifying the staffing mix in hospitals is by identifying budgeted Nursing Care Hours per Patient Day. A traditional measure of nursing productivity, "nursing hours per patient day has never been satisfactory because 'patient day' as a measure of nursing output takes neither patient acuity nor quality of nursing care into accou nt". .
The CalNOC data are less widely dispersed than the OSHPD data for the matched set of hospitals, suggesting that the CalNOC data might contain less measurement error. Nursing hours were on average higher in the OSHPD data than in CalNOC, likely because OSHPD data include nurse staff time spent on activities other than patient care. As a result, the distribution of nurse staffing per patient day is different between these datasets, with the CalNOC data producing somewhat lower hours per patient day than the OSHPD data. The correlations between estimates of hours per patient day are low, at 0.22 for total nursing hours and 0.32 for RN hours. Table 2 summarizes the critical care and medical–surgical nurse staffing and patient days data reported by CalNOC and OSHPD. OSHPD reports a greater number of RN and LPN hours as well as patient days, and all differences are statistically significant.
The greater number of nursing hours reported by OSHPD is consistent with OSHPD's productive hours including non-direct-patient-care hours, which may include RNs in special roles such as clinical specialists or infection control managers. The correlations between RN hours, LPN hours, and patient days are relatively high, ranging from 0.73 to 0.92. The correlations are higher for critical care than for medical–surgical care. It's been recommended that care hours per patient day be utilized as a staffing and productivity standard.
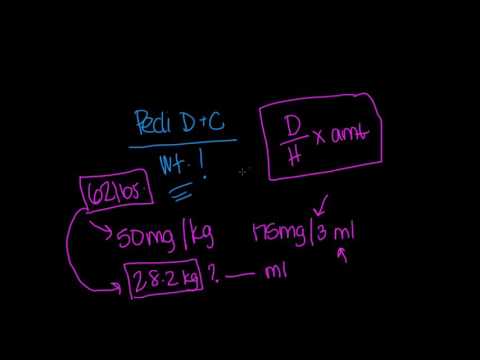
This method addresses nurse-patient ratios versus HPPD, capturing the acuity and actual care hours required to manage specific patient populations by encompassing all care hours and including all support staff. To ensure the optimal use of staffing resources, we must use standardized benchmarks and quality indicators, including patient and staff satisfaction. We must also consider productive and nonproductive hours , as well as the cost of incremental overtime. Currently, the Nursing Care Hours per Patient Day formula is the unit of analysis that determines staffing requirements in hospitals. It is a calculable formula that is used as a method of staffing and for budgeting nursing hours . Nursing Care Hours per Patient Day are calculated by multiplying the number of staff delivering direct nursing care by the hours worked during the shift and then dividing that number into the average daily census at a specific designated time.